As infectious organisms proliferate, some acquire genetic changes. Occasionally these allow an organism to become resistant to a particular treatment. When that treatment is given, the resistant microbes can continue to grow in our bodies, replacing the treatment-sensitive organisms. Resistance is more likely to develop when people do not take a full course of treatment, such as an antibiotic course.
Over time a drug-resistant strain of a disease can become the predominant strain in the community. When more than one type of treatment for an infection is available, a strain of microbes resistant to one treatment may be sensitive to another.
Over time, multi-drug resistance can develop, rendering many treatments ineffective. Increasing rates of multi-drug resistance are limiting the options for treating many types of infection, including malaria and tuberculosis.
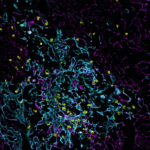
Our researchers aim to develop new treatments for infections using approaches that minimise the likelihood of resistance developing. By investigating the basic biology of infections, they are revealing how drug resistance occurs, and designing treatment strategies that are more difficult to evade.
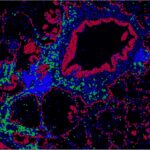
Treatments that boost the immune system’s clearance of infections are another approach that may overcome problems posed by multidrug resistant infections.