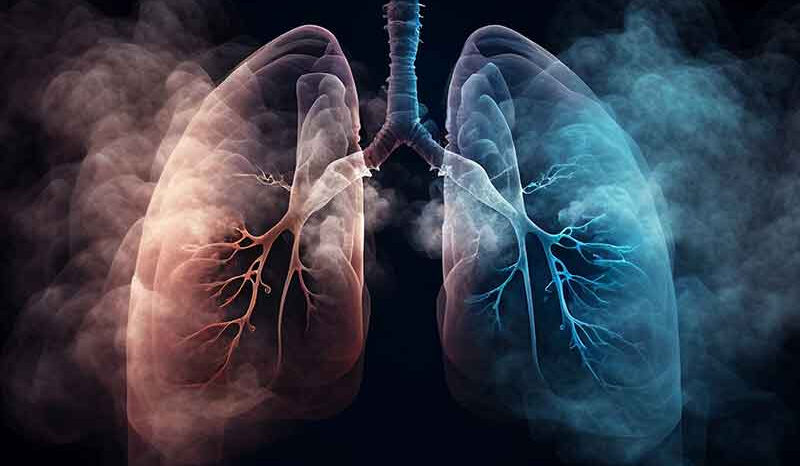
Lung cancer is a devastating disease causing 1.8 million deaths worldwide every year. Immunotherapy is a type of treatment that increases the elimination of tumour cells by an individuals own immune cells. Immunotherapy has dramatically improved the survival of many lung cancer patients. However, only a small proportion of patients respond to this type of therapy.
To identify new ways to improve response to immunotherapy, we need a comprehensive understanding of the communication between tumour and immune cells. The Asselin-Labat laboratory uses novel approaches that integrate spatial information with molecular characterisation and genomic screening to achieve this goal.
Our research focuses on studying the lung epithelium and the role of surrounding immune cells in maintaining lung health and controlling lung cancer formation. We work with preclinical models as well as clinical samples to assess the role of immune cells in maintaining lung homeostasis. We investigate mechanisms developed by tumour cells to escape immune surveillance. Our aim is to identify ways to reactivate immune activity against cancer cells with the ultimate goal to improve outcomes for people with lung cancer.
https://youtu.be/GGefqXNWW9g
3D OPT imaging showing Keratin 5 expression in Ezh2 cKO embryonic lung