Beating cancer with our immune system and new vaccines
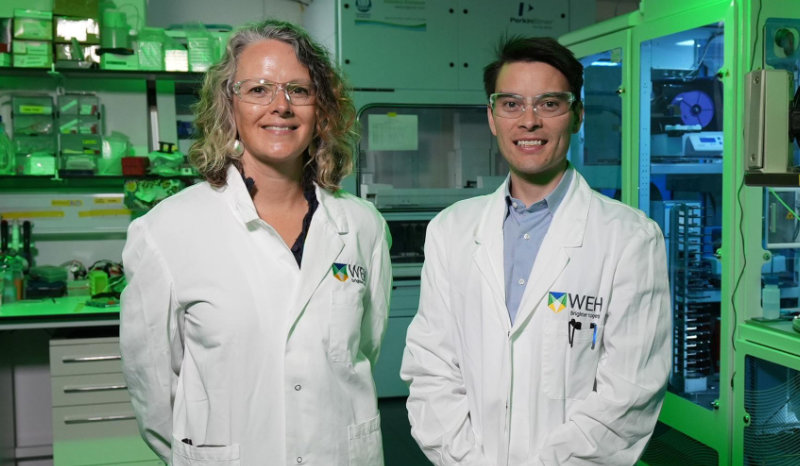
Professor Marie-Liesse Asselin-Labat’s team will investigate how cancer evades our immune system to uncover how immunotherapies and vaccines can be made more effective.
Immunotherapies have revolutionised cancer treatment. Why do only some patients respond positively to these treatments?
This is the big question in the field and what we are hoping to help address in this grant.
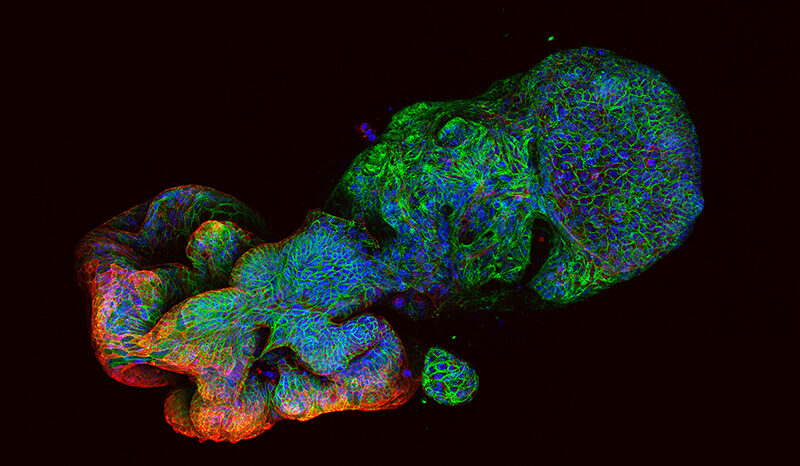
There are multiple factors necessary to have a good immune response against cancer cells during treatment with immunotherapy. For example, immune cells need to be able to both get into the tumour and recognise tumour cells as ‘bad cells’ to be eliminated.
Tumour cells utilise a number of ways to avoid being targeted and destroyed by the immune system, and we are hoping to understand what those are and how we can develop therapies to improve immune response against cancer.
What is your team hoping to understand about T cells, that will help improve immunotherapies for cancer?
T cells are a type of immune cell that orchestrates the body’s immune response, helping fight infection and disease. We hope to understand how to activate T cells that attack tumour cells, but also how we can inactivate a subset of T cells, called regulatory T cells, that prevent other T cells being active against the tumour.
One of the big challenges is that T cells activated by immunotherapy become ‘exhausted’. We need to understand the molecular mechanisms responsible for this exhaustion, so we can prevent or revert it.
What role could mRNA vaccines play in future cancer treatments?
There is a lot of excitement around mRNA vaccines for cancer treatment.
There are some studies in melanoma showing a positive response to cancer vaccines and ongoing clinical trials by BioNtech and AstraZeneca in lung cancer. These are therapeutic vaccines, not prophylactic vaccines like the ones we have for flu or COVID-19.
However we have little understanding of how the immune system and cancer cells will respond and adapt to cancer vaccines.
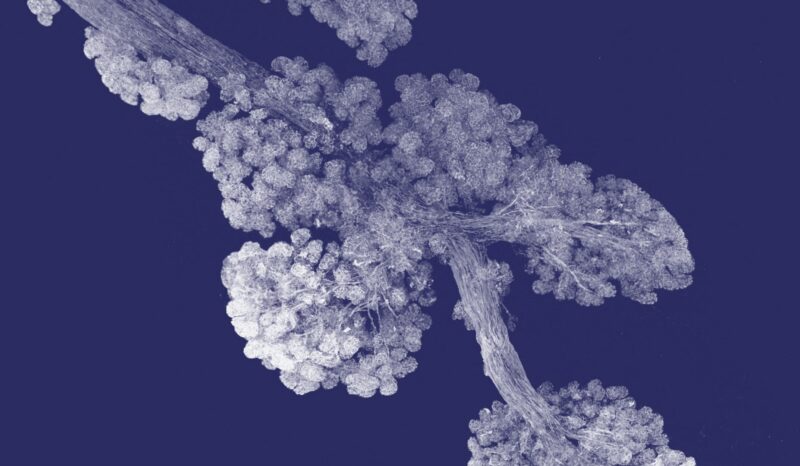
By understanding in detail the cellular response to cancer vaccines we hope to be able to develop a more efficacious and long-lasting vaccine. Our team will also work on developing a better formulation for vaccines so they are more effective and less toxic.
Looking forward five years to the end of this project, what do you hope to have found?
By the end of the five years, we hope to have a deep understanding of tumour and immune cell behaviours in response to immunotherapies, including cancer vaccines. We hope the research will identify novel therapeutic targets to boost the immune system against cancer cells and facilitate the access of immune cells inside the tumour to induce tumour cell killing.
‘Identifying and overcoming mechanisms of immune evasion in cancer’ is led by WEHI in partnership with the Peter Doherty Institute for Infection and Immunity, Monash University, Olivia Newton John Cancer Research Institute and Austin Health.