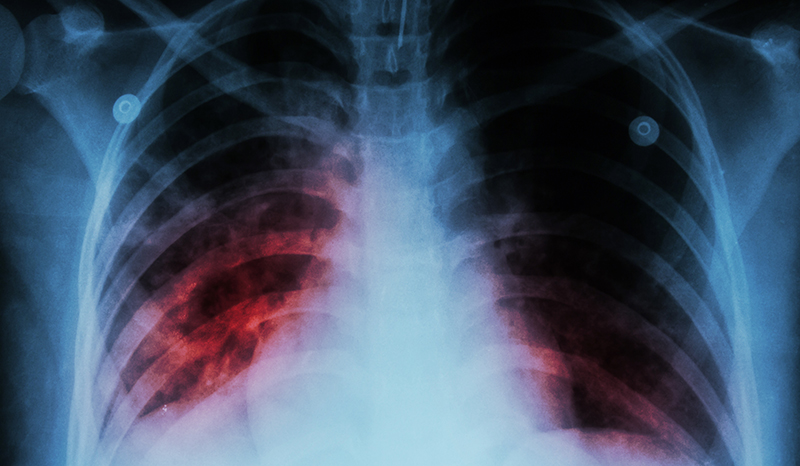
Macpherson L, Kik SV, Quartagno M, Lakay F, Jaftha M, Yende N, Galant S, Aziz S, Daroowala R, Court R, Taliep A, Serole K, Goliath RT, Davies NO, Jackson A, Douglass E, Sossen B, Mukasa S, Thienemann F, Song T, Ruhwald M, Wilkinson RJ, Coussens AK, Esmail H, Barry CE, Ellner JJ, Flynn JL, Heinsohn T, Horsburgh CR, Jacobson KR, Malherbe ST, Salgame P, Sheerin D, Streicher E, Tlala M, Via LE, Walzl G, Warren R, Warwick J. Diagnostic Accuracy of Chest X-ray Computer-Aided Detection Software for Detection of Prevalent and Incident Tuberculosis in Household Contacts. Clinical Infectious Diseases. 2025;80(3):10.1093/cid/ciae528
Munro JE, Coussens AK, Bahlo M. TBtypeR: Sensitive detection and sublineage classification of Mycobacterium tuberculosis complex mixed-strain infections. Communications Biology. 2025;8(1):10.1038/s42003-025-07705-9
Auld SC, Barczak AK, Bishai W, Coussens AK, Dewi IMW, Mitini-Nkhoma SC, Muefong C, Naidoo T, Pooran A, Stek C, Steyn AJC, Tezera L, Walker NF. Pathogenesis of Post-Tuberculosis Lung Disease: Defining Knowledge Gaps and Research Priorities at the Second International Post-Tuberculosis Symposium.American Journal of Respiratory and Critical Care Medicine. 2024;210(8):10.1164/rccm.202402-0374so
Coussens AK, Zaidi SMA, Allwood BW, Dewan PK, Gray G, Kohli M, Kredo T, Marais BJ, Marks GB, Martinez L, Ruhwald M, Scriba TJ, Seddon JA, Tisile P, Warner DF, Wilkinson RJ, Esmail H, Houben RMGJ, group ICFET, Alland D, Behr MA, Beko BB, Burhan E, Churchyard G, Cobelens F, Denholm JT, Dinkele R, Ellner JJ, Fatima R, Haigh KA, Hatherill M, Horton KC, Kendall EA, Khan PY, MacPherson P, Malherbe ST, Mave V, Mendelsohn SC, Musvosvi M, Nemes E, Penn-Nicholson A, Ramamurthy D, Rangaka MX, Sahu S, Schwalb A, Shah DK, Sheerin D, Simon D, Steyn AJC, Anh NT, Walzl G, Weller CL, Williams CM, Wong EB, Wood R, Xie YL, Yi S. Classification of early tuberculosis states to guide research for improved care and prevention: an international Delphi consensus exercise. The Lancet Respiratory Medicine. 2024;12(6):10.1016/s2213-2600(24)00028-6
Chambers ES, Cai W, Vivaldi G, Jolliffe DA, Perdek N, Li W, Faustini SE, Gibbons JM, Pade C, Richter AG, Coussens AK, Martineau AR. Influence of individuals’ determinants including vaccine type on cellular and humoral responses to SARS-CoV-2 vaccination. npj Vaccines. 2024;9(1):10.1038/s41541-024-00878-0
Savulescu AF, Peton N, Oosthuizen D, Hazra R, Rousseau RP, Mhlanga MM, Coussens AK. Quantifying spatial dynamics of Mycobacterium tuberculosis infection of human macrophages using microfabricated patterns. Cell Reports Methods. 2023;3(11):10.1016/j.crmeth.2023.100640
Sheerin D, Abhimanyu, Peton N, Vo W, Allison CC, Wang X, Johnson WE, Coussens AK. Immunopathogenic overlap between COVID-19 and tuberculosis identified from transcriptomic meta-analysis and human macrophage infection. iScience. 2022;25(6):10.1016/j.isci.2022.104464
Houben RMGJ, Esmail H, Cobelens F, Williams CML, Coussens AK. Tuberculosis prevalence: beyond the tip of the iceberg. The Lancet Respiratory Medicine. 2022;10(6):10.1016/s2213-2600(22)00184-9
Waters R, Ndengane M, Abrahams M-R, Diedrich CR, Wilkinson RJ, Coussens AK. The Mtb-HIV syndemic interaction: why treating M. tuberculosis infection may be crucial for HIV-1 eradication. Future Virology. 2020;15(02):10.2217/fvl-2019-0069
Seddon JA, Chiang SS, Esmail H, Coussens AK. The Wonder Years: What Can Primary School Children Teach Us About Immunity to Mycobacterium tuberculosis?. Frontiers in Immunology. 2018;9:10.3389/fimmu.2018.02946