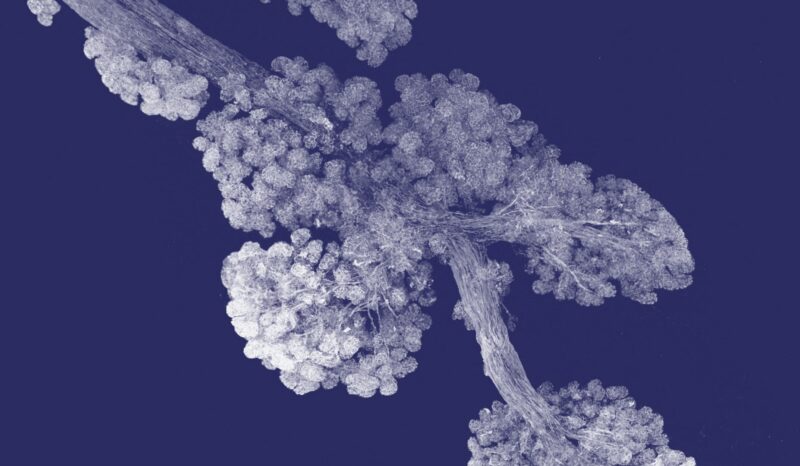
Extracellular vesicles (EVs) are like small delivery trucks that are dispatched by our cells to distribute important materials like proteins, fats and genetic information to other cells.
This delivery system helps cells communicate with each other, especially when they are under stress or dying.
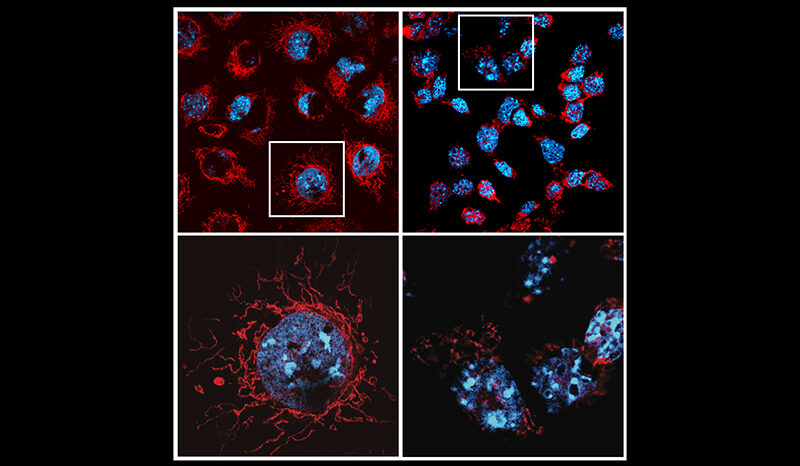
Research into how EVs form and their link to disease progression is challenging because of their small size, with most studies restricted to a ‘cells-in-a-dish’ approach.
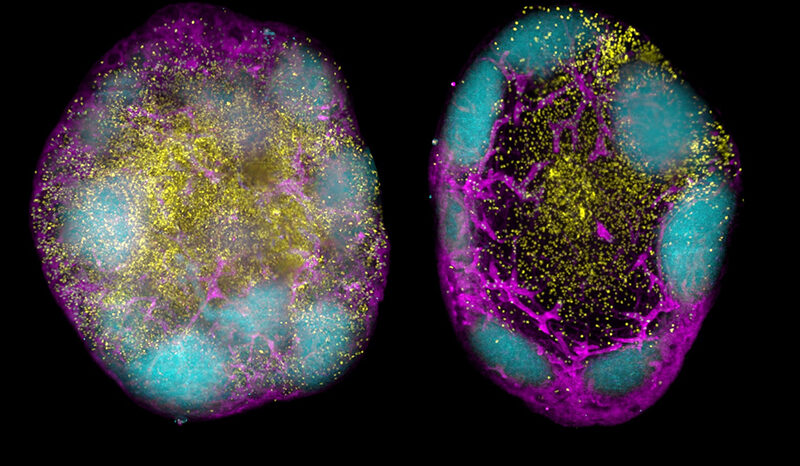
In an unprecedented study, researchers were able to overcome this significant barrier by imaging live EVs inside the bone marrow of mice.
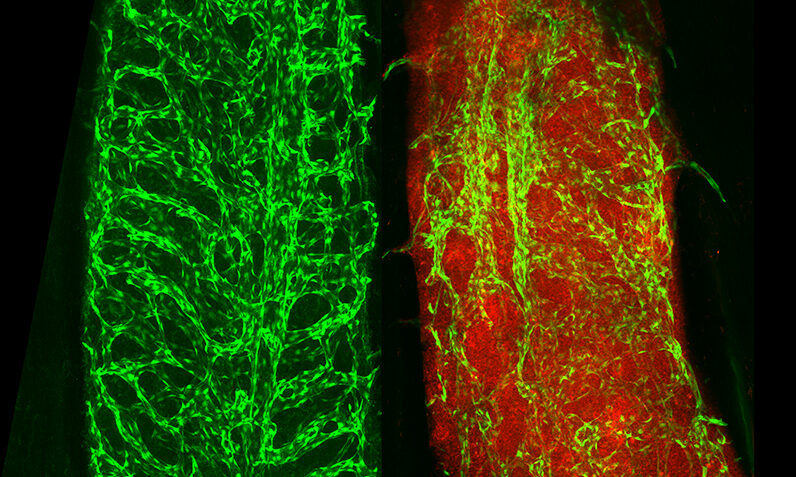
First author and WEHI cell biologist, Dr Georgia Atkin-Smith, said the team used high-resolution microscopy that can see directly inside the bone marrow of live organisms to capture the formation of EVs from blood vessels.
“No other study in the world has been able to achieve this so it’s a huge win for Australia’s scientific community,” Dr Atkin-Smith said.
“In this study, we’ve shown that the development of leukemia can degrade healthy blood vessels in the bone marrow. Mice with extensive blood vessel damage in their bone marrow had elevated levels of EVs in their blood, while healthy mice did not.
“This revealed – for the first time – that there is a link between EVs in the blood and tissue damage during cancer.
The potential link between EVs and blood vessel damage was first hypothesised in 2018 by senior author and WEHI Laboratory Head, Associate Professor Edwin Hawkins, who is an expert in ‘in vivo imaging’ – techniques that allow researchers to see inside living organisms.
“To have seen how the process of EV formation occurs with our own eyes after four years of research was an incredible moment,” Dr Atkin-Smith said.
“Pictures tell a thousand words, and these ones have significantly advanced our understanding into EVs by showing how they form under both healthy settings and during disease.
“This has not only developed a new framework to study the formation of EVs in model organisms, but could inform new diagnostic tools to monitor the level of tissue damage observed during disease through a simple blood test. It’s an incredibly exciting advancement.”