Professor Don Metcalf, described as the father of modern haematology, begins his research career at the institute.
He discovers colony stimulating factors (CSFs), the hormones that boost infection-fighting white blood cells in the body. The discovery goes on to help more than 20 million cancer patients worldwide recover from chemotherapy and revolutionises blood stem cell transplantation.
20 million lives
Reflecting on his life’s work in an interview in 2005, Metcalf characterised the discovery that sparked his epic 40-year quest as an accident.
The moment – in 1965, when Dr Ray Bradley, a young scientist at the University of Melbourne, crossed Royal Parade to show Metcalf a thriving colony of cells he had grown in a Petri dish – is etched in Walter and Eliza Hall Institute lore.
But the circumstances that turned this bit of luck into therapies that would benefit 20 million lives – and counting – were no accident. They were the product of visionary contrivance, intersecting with Metcalf’s brilliance and single-minded endurance.
Early support for cancer research
The groundwork was laid a decade earlier by Dr EV ‘Bill’ Keogh, an “enigmatic behind-the-scenes mover and shaker in medical circles”, to borrow the insight of Sir Gustav Nossal, and a mentor to many young talents.
Keogh, head of what was then the Anti-Cancer Council of Victoria, had secured a benefactor whose donation would create a fellowship to support cancer research. Casting around for a suitable candidate, he asked his friend at the University of Sydney – bacteriologist Professor Hugh Ward – to nominate someone “young and smart … and he approached me”, Metcalf would recall.
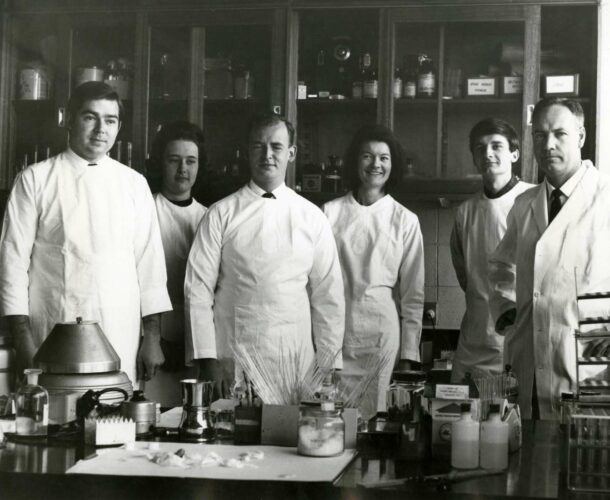
So it was that Metcalf, the precociously gifted middle child of country schoolteachers who started school, aged 3, in grade 2; university at 16; landing in Melbourne as the Carden Fellow in 1954, at 25. Bankrolled by the fellowship, as he would be for his entire career, Metcalf was installed in the Walter and Eliza Hall Institute.
Working under Burnet
Metcalf’s first inauspicious encounter with the institute’s director, lauded virologist and soon-to-be Nobel Prize-winning immunologist, Sir Frank Macfarlane Burnet, set the tone for a personally testy albeit professionally respectful relationship.
Burnet declared that “cancer was inevitable, and that there was no point doing research about what caused it – it just happened, and there was no cure other than surgery”, Metcalf recalled. “So there was no point doing research – if you did it you were either a fool or a rogue.” (Cancer would ultimately claim both their lives – Burnet in 1985, of colon cancer; Metcalf in 2014, of pancreatic cancer.)
Burnet instructed Metcalf to spend two years working in virology. Only then might he pursue cancer. Metcalf served the time, and then went to refine his cancer understanding at Harvard.
On returning to the institute in 1958, Metcalf found himself allocated rooms in the bowels of the Royal Melbourne Hospital, perched above the institute’s “rather large and smelly animal house”, says Nossal.
Working under Nossal
In 1965, when Nossal succeeded Burnet as director, he repatriated Metcalf to a whole floor of the expanded institute. He also made Metcalf assistant director, explaining in his book Diversity and Discovery that he “considered him to be the best and most original scientist on the staff, and also because his personality was so different from my own.
“My exuberance, pomposity and naïve optimism found a foil in his sobriety, solid determination and iconoclasm … This may have been the best decision I ever made.”
Around this time Ray Bradley, working at the university, was experimenting with the techniques bacteriologists used to culture bugs in dishes of agar and spawned a thriving crop of cells from a single bone marrow cell. Something was at play promoting the growth of these cells, but what was it?
The start of the CSFs story
This was the question Bradley took to Metcalf. “We wondered whether these were the hormones that we knew the body must use to control the production of blood cells,” Metcalf recalled many years later. “You make enormous numbers of them every day, and you have to control this very carefully.
Nobody knew what these were, so we had to discover them. That took us about 10 years.” They identified four “colony stimulating factors”, or CSFs. These are the hormones that controlled the growth, behaviour, work and longevity of powerful blood cells, the ones that “protect you from bacterial and fungal infections – that will keep you alive tomorrow if you get an infection like that.
The next step was to purify these hormones, but they exist in such tiny quantities it took another 15 years to yield enough to test them in culture dishes. “Then we had to figure out how to mass produce them so we had enough to test in animals or even test in humans,” Metcalf explained. “And the way you do that is to find the genes that code for those hormones and put them into bacteria or yeast and mass produce the product in big fermentation tanks.”
The initial source was human urine, available in plentiful amounts – collected in buckets in the institute’s men’s urinals, with donations spiking on a Friday evening after a trip to the pub. Hundreds of litres of urine were processed to capture microscopic samples of pure CSFs.
Then it was discovered that the hormones could be captured in better quality and quantity from the lungs of mice, processed in batches of 800 at a time. Still, “it took 20 years before we had enough stuff to test in the first mouse. Yes it did work – great, we should get the same results in humans,” Metcalf recalled.
Another two years, and the FDA (Food and Drug Administration) in America licenced two of the four CSFs for clinical use.
CSFs used to treat cancer patients
Unfortunately while Metcalf and his collaborators at the Walter and Eliza Hall Institute garnered scientific and academic glory, they were creatures of a more innocent age of experimentation and didn’t win the race to the patent office for the blockbuster therapies derived from G-CSF. Metcalf’s name was on the GM-CSF patent, however, “which, though not a huge seller, made very nice royalties both for the institute and for Don himself as the inventor”, Nossal says.
Today it is estimated that some 20 million cancer patients have benefited from CSFs, which are routinely used to help patients survive the rigours of chemotherapy. New applications in fighting a wide range of diseases are constantly emerging.
Treating Jose Carreras
One of the first people to benefit from CSFs was the celebrated tenor Jose Carreras. He became part of a CSF trial after he was diagnosed with acute leukemia. “The treatment for that is massive doses of chemotherapy that kill your entire bone marrow cells, and then you have a transplant of bone marrow cells from a donor which hopefully regrows quickly,” Metcalf explained in his interview marking the institute’s 90th anniversary.
But Carreras’ transplant failed, “so he was left for three months without any white blood cells, unprotected from infections, and in a very parlous state of health. He happened to be one of the first people given the CSFs we had grown and mass produced.”
Interviewer Louise Darmody asked Metcalf in 2005 if he had saved the singer’s life. “I think so, yes.” Carreras certainly thought so. He came to Melbourne to sing happy birthday to Metcalf, and invited the music lover to the opera several times as a guest.
There’s always more work
Darmody observed that it must be a wonderful feeling, to save so many lives. It’s satisfying, Metcalf agreed, but “that doesn’t solve tomorrow’s problems”. There’s always more work, though he did concede that “probably, the most important thing is to have done something useful.”
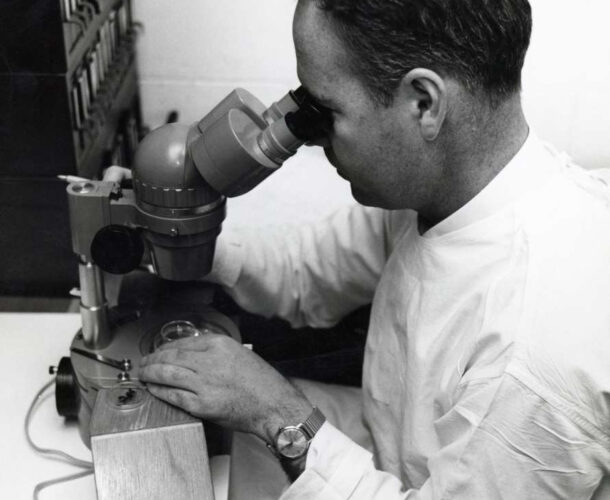
Metcalf officially retired in 1996 but continued to work six days a week until late in 2014, when his health failed. Why? What drove him?
Being part of a team was a big component. “It’s fun to come to work in the morning, because somebody will be running hot, somebody will be in the gloom.
“And the questions you are asking are so complicated that it makes chess look an idle pursuit, and you can’t think of anything else that it is more interesting to do.
“The fact that if you came in and looked at me I would be sitting counting colonies [under the microscope] as I have been counting for 30 years, you would say that is incredibly boring. But what I’m doing is thinking about what it all means as I am counting. So it is a strange combination of having endless, repetitive, apparently boring things to do and not having a dull moment doing it.
I’m a doctor. And I know very well that down the corridor there are people who are dying. And you are involved in a pretty serious matter of life and death. And so for me, as distinct from scientific colleagues I have, I’d like to discover more cures for diseases that are actually down the corridor.
A sad goodbye
Metcalf died on 15 December 2014, survived by his wife Josephine – an “intelligent, bright, witty” nurse who he met soon after arriving in Melbourne – their four daughters, and six grandchildren.
He was remembered by his colleagues “for his formidable work ethic and exacting scientific observations to the point of obsession.
“Don was brutally honest with a dry wit and had little tolerance for work he considered superficial.” At the same time many young researchers fondly recall his interest in, and encouragement of, their work.
“Don Metcalf was a scientist with rare insight and great foresight. We will miss him dearly,” his obituary concluded.