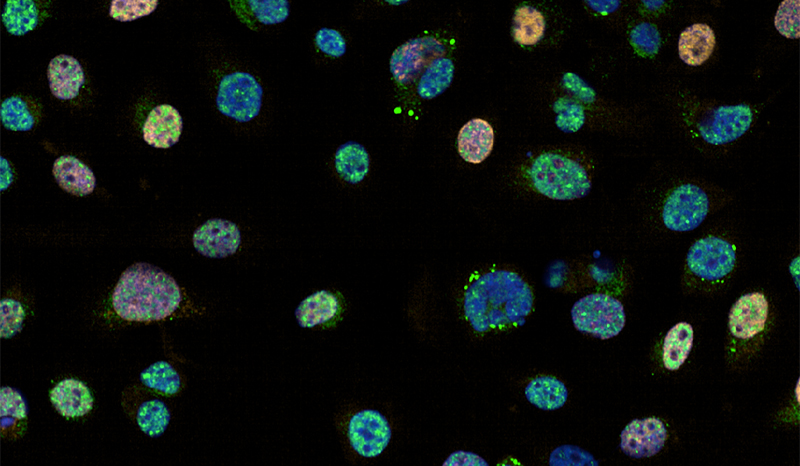
Breast cancer arises from cells within the breast that accumulate changes to their DNA (‘genetic mutations’) that make them grow in an uncontrolled manner.
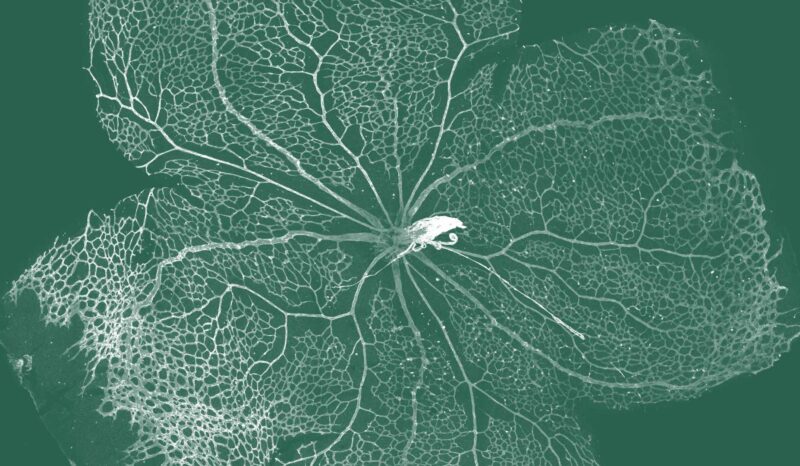
The structure of the breast is designed to produce and secrete milk from the nipple. Most breast cancers arise from cells in the breast ducts, which normally transport milk to the nipple. Some cancers develop from cells in the milk-producing lobules. It is rare for cancers to come from other structures in the breast such as fat or lymphatic vessels.
Breast cancers begin as a small, confined tumour, but can grow and spread throughout the breast. Early growths that are ‘pre-invasive’ as they have not left the ducts are termed DCIS (for ‘Ductal Carcinoma In Situ’). Invasive cancers are often described as ductal or lobular, based on their appearance down the microscope.
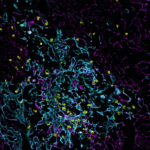
Some breast cancer cells may develop further changes that allow them to escape from the breast. They travel through lymphatic vessels to lymph nodes, or spreading through the blood to other organs, a process called ‘metastasis’.