Of the 13,000 Australians diagnosed with lung cancer every year, 10% of men and 35% of women have no history of smoking.
The new research, published in Cancer Cell, was co-led by WEHI Associate Professor Marie-Liesse Asselin-Labat and Professor Daniel Gray.
Associate Professor Asselin-Labat said differences in the immune reactions between smokers and non-smokers may explain why only 20% of patients with lung cancer responded to immunotherapy treatment.
“It shows that we need to take a different approach to treating smoker and non-smoker patients with lung cancer,” she said.
“In smokers, we need to make the tumours visible to the immune system for immunotherapy to be effective, whereas in non-smoker patients we need to activate a dormant immune system to enable it to fight the tumour.”
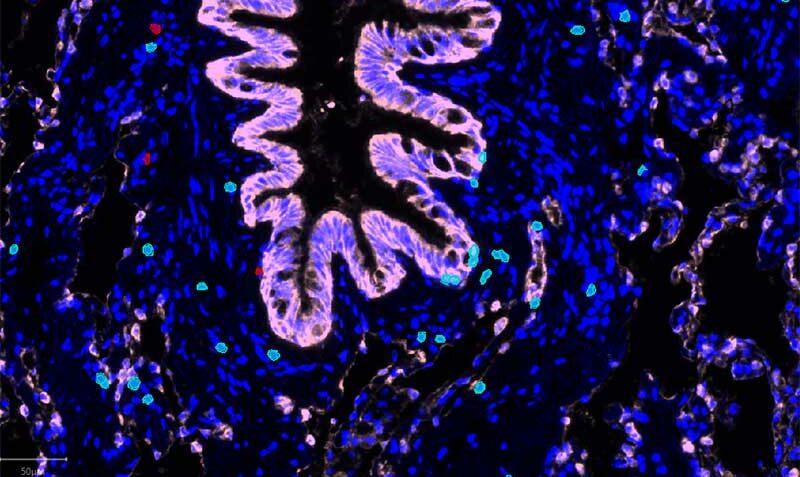
Professor Gray said the research teams had made interesting observations about the environment in which tumours grow and the difference in disease progression between smokers and non-smokers.
“There’s a very different inflammatory environment in the lungs of smokers compared to those who had never smoked,” he said.
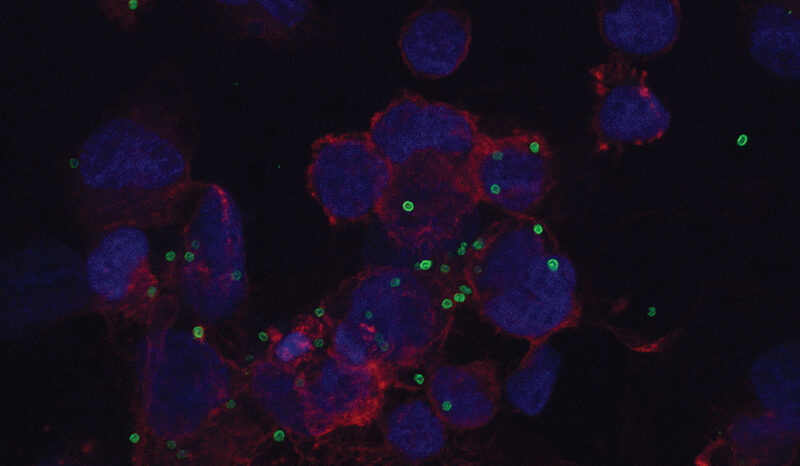
“We found a specific subset of T cells, called TRM, that are highly enriched in smokers. In these patients, the TRM apply pressure on the tumour to evade the body’s immune response.
“Immunotherapy is less effective against tumours that acquire this property.”