Cells can die because they are damaged, but most cells die by killing themselves.
There are several distinct ways in which a cell can die. Some occur by an organised, ‘programmed’ process. Some cell death processes leave no trace of the dead cell, whereas others activate the immune system with substances from the dead cell.
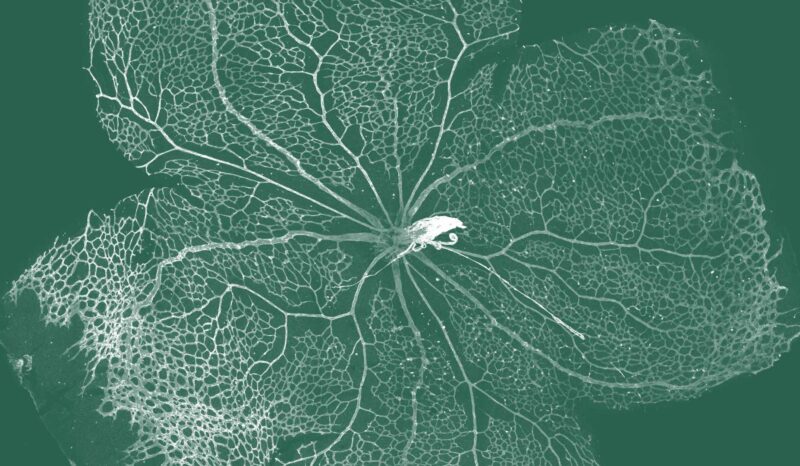
Apoptosis: is a form of cell death that prevents immune activation. Apoptotic cells have a particular microscopic appearance. The cell activates proteins called caspases that are normally dormant. These caspases dismantle the cell from within. The apoptotic cell breaks into small packages that can be engulfed by other cells. This prevents the cell contents leaking out of the dying cell and allows the components to be recycled.
Necrosis: occurs when a cell dies due to lack of a blood supply, or due to a toxin. The cells’ contents can leak out and damage neighbouring cells, and may also trigger inflammation.
Necroptosis: is similar in appearance to necrosis, in that the dying cell’s contents can leak out. However, like apoptosis, necroptosis is a programmed suicide process triggered by specific proteins in the dying cell.
Pyroptosis: is a form of cell death that occurs in some cells infected with certain viruses or bacteria. A cell dying by pyroptosis releases molecules, called cytokines, that alert neighbouring cells to the infection. This triggers inflammation, a protective response that restricts the spread of the viruses and bacteria.