The gluten-free diets of Australians with coeliac disease will be scrutinised through two studies being undertaken at the Walter and Eliza Hall Institute of Medical Research.
Coeliac disease is an autoimmune condition caused by gluten, a food protein found in wheat, rye, barley and oats. The disease often causes digestive symptoms such as bloating, abdominal pain and diarrhoea. It can also cause anaemia, low iron levels and excessive tiredness. One in 60 women and one in 80 men in Australia have coeliac disease but 80 per cent remain undiagnosed.
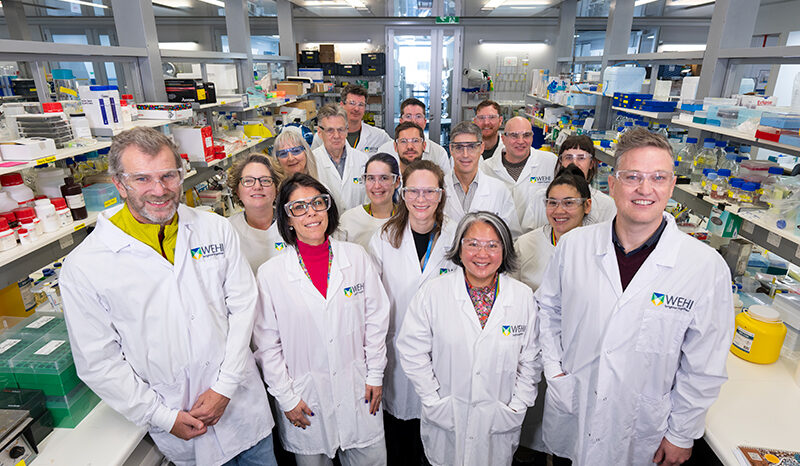
In one study the Institute’s coeliac disease research team, led by gastroenterologist Dr Jason Tye-Din, will examine the safety of oats for people with coeliac disease. In the second study the team will investigate why half of all Australian adults with coeliac disease fail to get full healing of their bowel or suffer symptoms even after many years on a gluten free diet.
The studies have been made possible through funding provided by Coeliac Australia.
Why does the gluten-free diet fail?
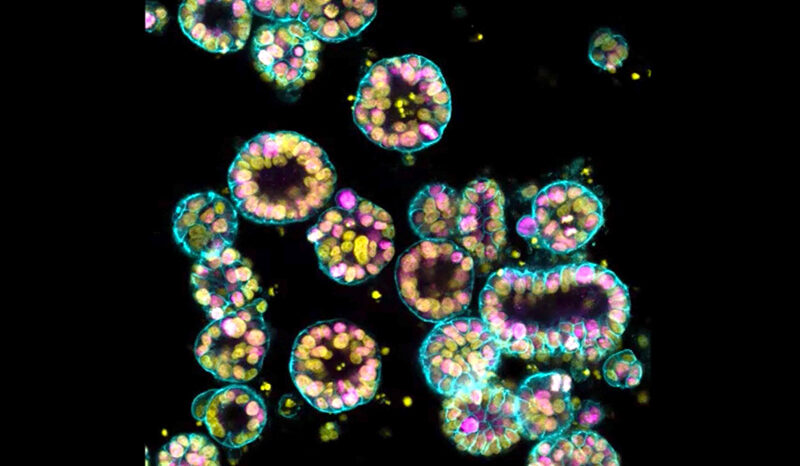
The gluten-free diet is the mainstay of treating coeliac disease yet half of all Australian adults with coeliac disease still experience disease symptoms or intestinal damage despite many years following the diet.
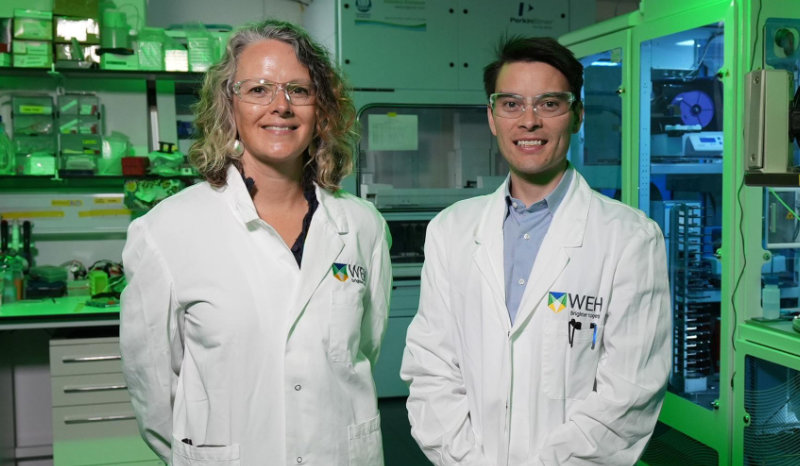
Specialist dietitian Dr Emma Halmos and the team are investigating the reasons why the gluten-free diet doesn’t always work as intended. She said the findings would be critical to improving the health of people with coeliac disease.
Some of the reasons being explored to explain the failure of the gluten-free diet are:
- Packaged food labelled as gluten-free actually containing gluten
- Food handling practices in food outlets that prepare and sell gluten-free foods
- Patient knowledge of and compliance with the gluten-free diet
- The accuracy of tests intended to measure gluten levels in food
“The cause of ongoing intestinal inflammation or symptoms in people with coeliac disease is often attributed to accidental or low amounts of gluten exposure but why this happens and what causes it is poorly understood,” Dr Halmos said. “Persistent intestinal inflammation due to inadequately treated coeliac disease is a major concern as it substantially increases the risk of complications such as other autoimmune diseases, osteoporosis, cancer and death.”
Determining the safety of oats in coeliac disease
Oats are a highly nutritious cereal but in Australia and New Zealand coeliac patients are encouraged to exclude them from their diet as they are potentially harmful to some coeliac patients.
Dr Melinda Hardy and the team will explore:
- Why some people with coeliac disease get sick when eating oats
- If there is a dose of oats that can be safely consumed by all coeliac patients
- Developing a food test to identify the unsafe parts of oats
Dr Hardy said findings from the study would help doctors manage patients and guide approaches that may enable oats to be safely reintroduced into the gluten-free diet.
People with coeliac disease interested in participating in either study should contact the Walter and Eliza Hall Institute’s coeliac research nurse Cathy Pizzey at coeliac@wehi.edu.au.