Parkinson’s disease is the fastest growing neurological disorder worldwide and second in prevalence to Alzheimer’s. Parkinson’s is neurodegenerative, meaning it will continue to get worse over time, and there is still no cure or drugs to slow or stop the progression of the disease.
The current best estimate is that more than 200,000 Australians live with Parkinson’s in Australia, with nearly 40 people diagnosed every day. Those figures are forecasted to double in the next 15 years. The exact number of people with Parkinson’s is not known as there is no clinical diagnostic test.
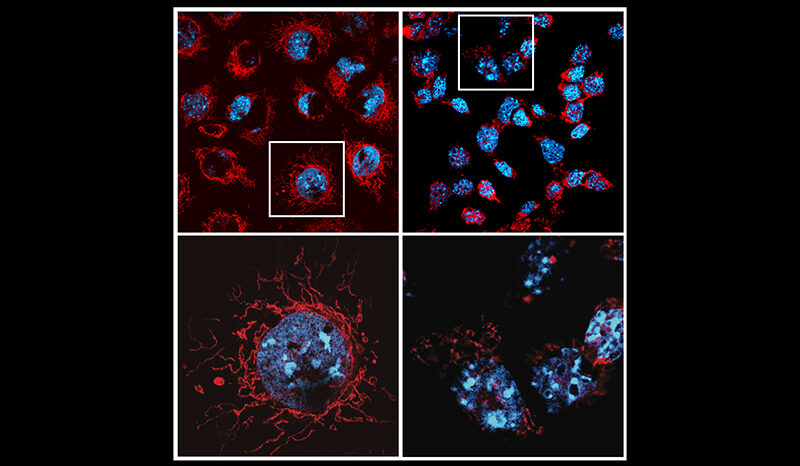
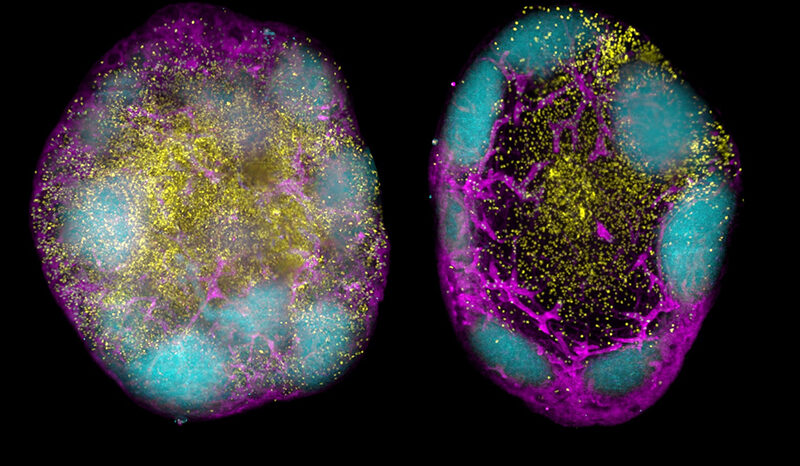
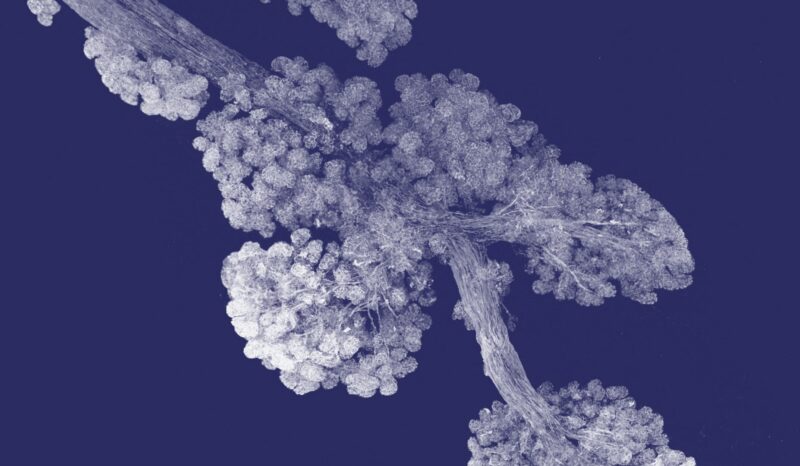
In a team effort spanning both the Bahlo and Dewson labs from the Parkinson’s Disease Research Centre as well as WEHI’s Human-based Research and Clinical Trials group and WEHI Research Computing, researchers led by Professor Melanie Bahlo and Dr Fei Wang discovered a new link between blood immune cells and Parkinson’s disease.
The finding brings the team a critical step closer to a blood test that could be used for diagnosing and monitoring the progression of the disease.
“The ultimate goal is to be able to screen for Parkinson’s disease in a similar way to the national screening program for bowel cancer, so people can get access to medication sooner,” Prof Bahlo said.