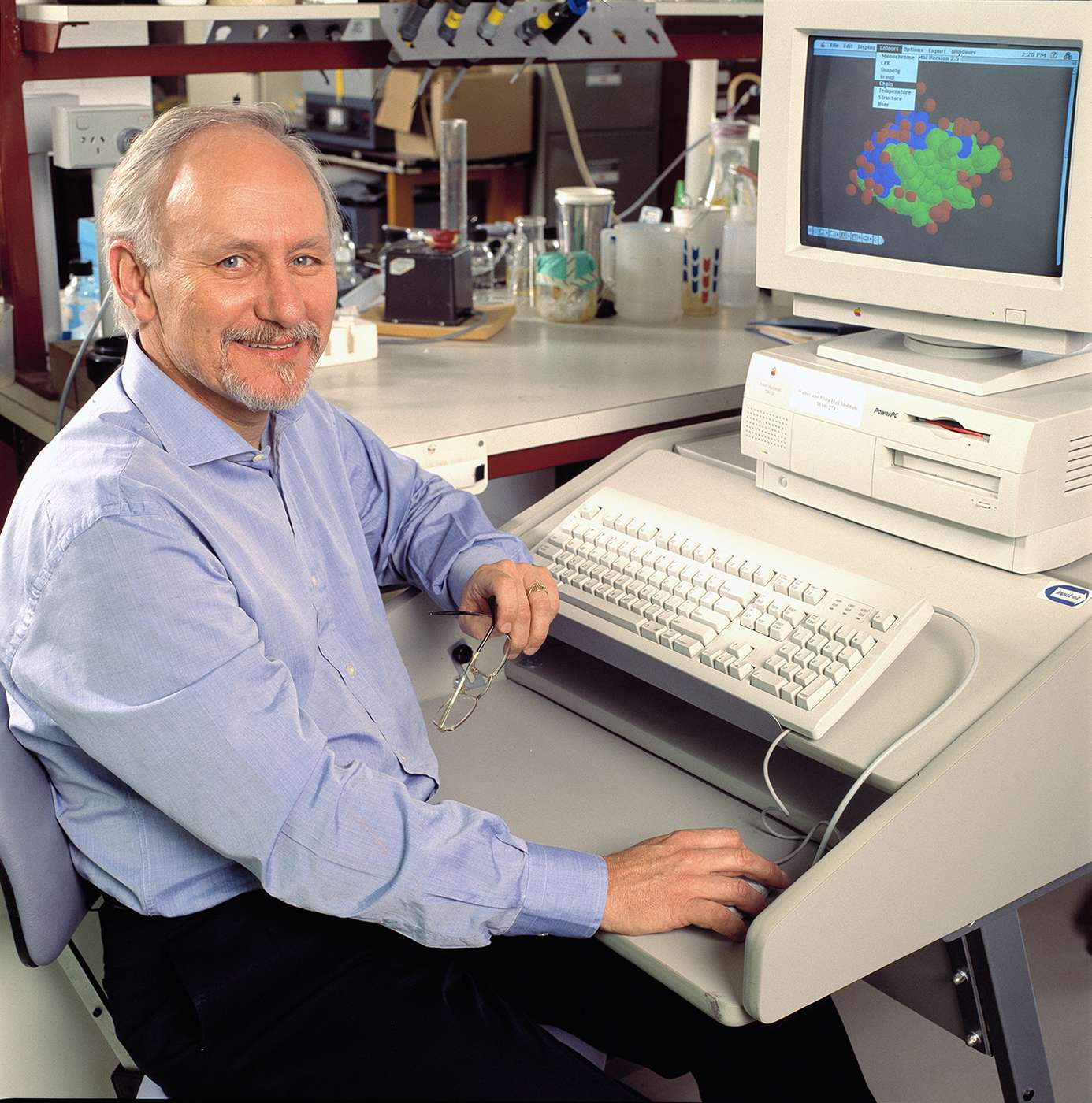
Professor Len Harrison and scientists from the Walter and Eliza Hall Institute provide the first evidence directly linking insulin to the development of type 1 diabetes.
Type 1 diabetes
Type 1 diabetes occurs when the immune system – and T cells in particular – attacks and destroys beta cells in the pancreas that produce the hormone insulin. Without insulin, the level of the sugar glucose in the blood cannot be controlled.
Almost all people with type 1 diabetes rely on insulin injections for their entire lives and, even with the best care, are at risk of complications such as kidney, eye, nerve and blood vessel damage, heart disease and stroke. Insulin was discovered in the early 20th century as an effective treatment for diabetes, by replacing the insulin that beta cells were no longer able to make.
Role of insulin in diabetes
However while insulin loss is the end of the story, it is also the beginning. In 1997, Harrison, Professor Andrew Lew and visiting scientist Michelle French provide the first direct evidence that insulin itself is an immune target that drives the development of type 1 diabetes. They show this in an animal model genetically predisposed to develop type 1 diabetes.
“The thymus is where T cells first ‘learn’ tolerance to the body’s own molecules,” Harrison says.
“T cells that react to self-antigens, such as insulin present in the thymus, are culled en masse to prevent autoimmune disease, but the process is not perfect and a few T cells get through.
“We wondered if boosting the amount of insulin in the thymus could improve the elimination of insulin-reactive T cells, that potential cause type 1 diabetes,” Harrison says.
The strategy proved very effective.
“In this mouse model, we could stop the development of diabetes virtually one hundred per cent.”
In their paper, the authors “conclude that autoimmunity to proinsulin plays a pivotal role in the development of IDDM.”
Evidence starts accumulating
Harrison and Peter G Colman from The Royal Melbourne Hospital later find in genetically at-risk babies followed from birth that the first indication of autoimmunity in type 1 diabetes is the presence of antibodies to insulin.
In 2003 Harrison, Steptoe and Ritchie from the institute program future antigen-presenting cells to express insulin in the thymus while T cells develop.
“This causes the self-reactive T cells to self destruct,” Harrison says. “It shows that deleting T cells that recognise and attack insulin can totally prevent development of diabetes.”
In 2005, Nakayama, Eisenbarth and colleagues at the University of Colorado Health Sciences Center, Denver, US, publish a Nature paper that pinpoints the part of the insulin protein that stimulates T cells to cause type 1 diabetes in the mouse.
From victim to weapon
“The evidence was accumulating that insulin was a key factor in diabetes developing,” Harrison says.
“Though the discovery was not directly translatable to humans, it gave us a good lead to shift our focus to insulin to induce tolerance. By now we had a solid idea of how we could tell if someone was at risk of developing type 1 diabetes. The next step was to turn the process on its head, to make insulin a tool not a target, to stop diabetes developing.”