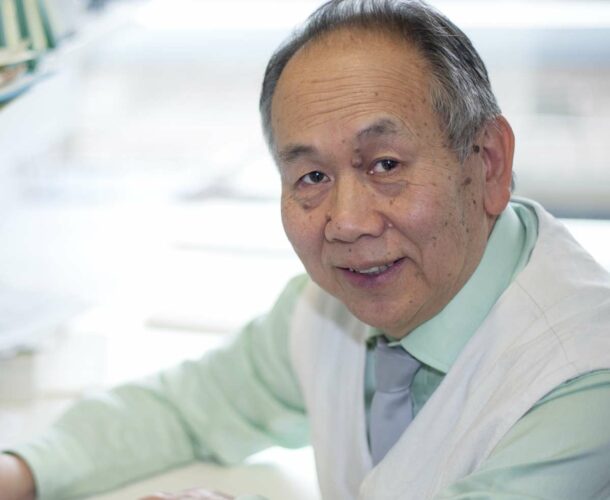
Professor Andrew Lew and his colleagues pool their resources to set up a new type 1 diabetes research program to look into the most important issues in type 1 diabetes, and how collaboration between diabetes researchers and immunologists might successfully address these.
A bright idea
One day in the early 1990s Professor Andrew Lew and his colleagues were brainstorming about diabetes in the light-filled tearoom at the Walter and Eliza Hall Institute.
Lew studied veterinary science at university before a PhD and subsequent fellowship led him to pure immunology. He and some other immunologists were chatting with researchers from the institute’s type 1 diabetes program, including Professor Len Harrison and Dr Tom Mandel, the Australian pioneer of islet transplantation, which remains the only cure for the debilitating disease.
“We were thinking ‘why not pool our resources and set up a type 1 diabetes program?’” Lew recalls. “There I was, an immunologist interested in diabetes research, but I hadn’t studied the disease. Conversely, type 1 diabetes tends to be seen as a metabolic disease but it’s also an immune disease because the immune system kills the islet cells in the pancreas that make insulin — few researchers see the two together.”
That day Lew and his colleagues asked: ‘what are the most important issues in type 1 diabetes research and how can we address them together?’
Transplants the key
The problem remains largely the same today as it was 20 years ago: how to stop a transplant recipient from rejecting the healthy islets, without shutting down their entire immune system.
Type 1 diabetes affects about 150,000 Australians — Lew points out that the numbers are rising in the developed world.
The disease strikes people in their youth, knocking out their ability to produce enough insulin for tissues like brain and muscle to take up sugar from their bloodstream. Keeping their blood sugar stable involves multiple insulin injections each day with potentially catastrophic consequences should their glucose levels go too high or too low. Patients also face the risk of long-term complications: such as blindness, kidney failure and poor circulation leading to leg amputation.
About a dozen transplants, where islets from human donors are placed into the liver, have been performed in Australia. The results are “brilliant,” Lew says. “About five of those patients are completely insulin independent now, they don’t need injections anymore. That’s as good a result as you’ll see anywhere in the world.”
What’s the catch?
There is a catch — several, in fact. The surgery is expensive, donors are scarce and the islets are difficult to harvest as the pancreas is a bag of enzymes that is “the first to disintegrate in a dead body; it literally chews itself up”.
Another big obstacle to the utilitarian potential of islet transplants is the administering of drugs to suppress immune rejection of the transplant.
“When you do islet transplants, you have to give patients these drugs to stop the rejection of the islets,” Lew explains, “and long-term these have some nasty side effects, with the person susceptible to infections and cancer, as the drugs themselves are toxic.
“So this means we have to weigh the burden of the immunosuppressive drugs against the burden of the disease.” It follows that the only suitable candidates for transplant surgery are those who struggle to sense that their blood sugar is plunging so low they fall into coma.
Guided missiles
The answer, according to Lew and his colleagues, is to better target the immune suppression — use a guided missile rather than an atom bomb.
“We thought, why not endow the islets themselves with the ability to suppress the immune system at the liver. Why not try to get the islets to secrete one of those blocking molecules — such as blocking antibodies — that tells the immune system, ‘don’t go any further, stop!’” That is, use the immune system to control itself.
Challenges and promise
As always, the challenge is securing funding for clinical trials. “That’s what’s missing. We don’t really have a biotech industry here, though things are changing slowly.”
Globally, however, immunology is a booming $50 billion market, “as the biggest blockbuster drugs are antibodies to fight cancer, rheumatoid arthritis, other diseases. We’re on the verge of understanding so many diseases through immunology.
“We can make an antibody to anything, which means theoretically we can mimic or block anything. Lew smiles. “There’s almost limitless potential.”