Professor Brendan Crabb and Professor Alan Cowman create the world’s first genetically modified malaria parasite. Using their new technique, they reveal how infected red blood cells stick to the walls of blood vessels.
Foreign DNA
Since scientists have been able to grow malaria parasites in the laboratory, they have attempted to ‘knock out’ specific genes to determine their function. Traditional techniques fail to work as the parasite’s DNA contains only one copy of each gene, so accidental deletion can be fatal for the parasite.
In the early 1990s, researchers had succeeded in inserting DNA from other organisms into the malaria parasite using a fragment of genes found in bacteria called a plasmid. However, this insertion did not become incorporated into the parasite’s DNA, and was soon bred out in subsequent generations of the parasite.
Targeted insertion
Crabb and Cowman’s revolutionary technique relies on this insertion of plasmids, but with a twist. They genetically engineer plasmids to insert a specific gene at a specific site of the parasite’s DNA. When inserted, it breaks an existing gene, rendering it inactive. The gene they insert comes from another parasite and gives the malaria parasite resistance to a drug that usually kills it. This allows Crabb and Cowman to test if their new technique has worked – if the gene has been inserted, the parasite won’t die when exposed to the drug – while examining what impact rendering the target gene inactive has on the parasite.
Sticky blood cells
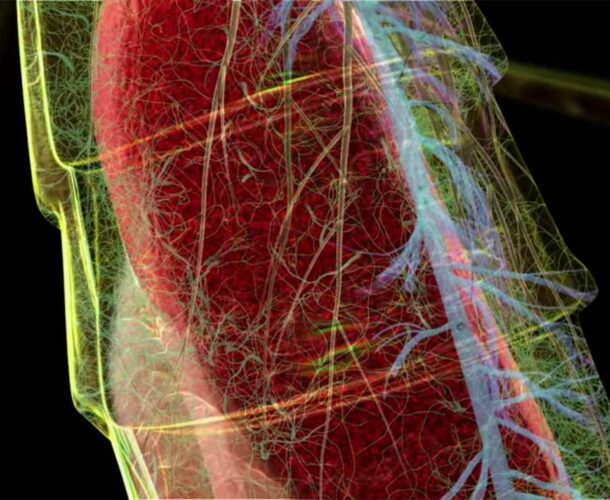
To demonstrate the power of their technique, Crabb, Cowman and colleagues engineer a plasmid that inserts the drug-resistance gene into the KAHRP gene which is thought to produce knobs on the surface of malaria-infected blood cells. They find parasites with disrupted KAHRP don’t produce knobs on the surface of infected blood cells and don’t stick to the side of blood vessels. Sticking to blood vessels is a key step in the progression of malaria and coincides with the development of symptoms of the disease.
The development of genetic modification techniques and the discovery that the KAHRP gene is required for infected blood cells to stick to the side of blood vessels underpins decades of research into malaria and enables the development of a potential vaccine.